Abstract
Introduction Diffuse large B-cell lymphoma (DLBCL) is the most common form of aggressive non-Hodgkins lymphoma, accounting for up to 40% of cases. Long term remission is achieved in 50-60% of the patients with rituximab and anthracycline based treatment, but the remaining patients will have either primary refractory or relapsed disease. Prior to the advent of CAR-T-cell therapy, salvage chemotherapy followed by autologous hematopoietic stem cell transplantation (ASCT) was the standard of care for these cases of relapsed or refractory (r/r) disease. For those who relapse post ASCT, options are limited and outcome was dismal. With the results of recent pivotal studies, CAR-T-cell therapy is now offered in patients who are not ASCT candidates and for those who relapse after ASCT. The phenotype of patients who proceed to CAR-T without ASCT is possibly different than those who are able to achieve a clinical response and then proceed to ASCT.
While numerous trials have compared the clinical outcomes of ASCT and CAR-T, few have investigated outcomes of CAR-T in previously transplanted versus transplant naïve patients. Wang et al. demonstrated a potential benefit for sequential ASCT and CAR-T in 14 patients with r/r DLBCL, with a median PFS of 14.82 months. Our study compared the clinical outcomes of previously transplanted and transplant naïve patients with r/r DLBCL who received axi-cel (Yescarta) CD19 CAR-T therapy at our center between 2018-2021.
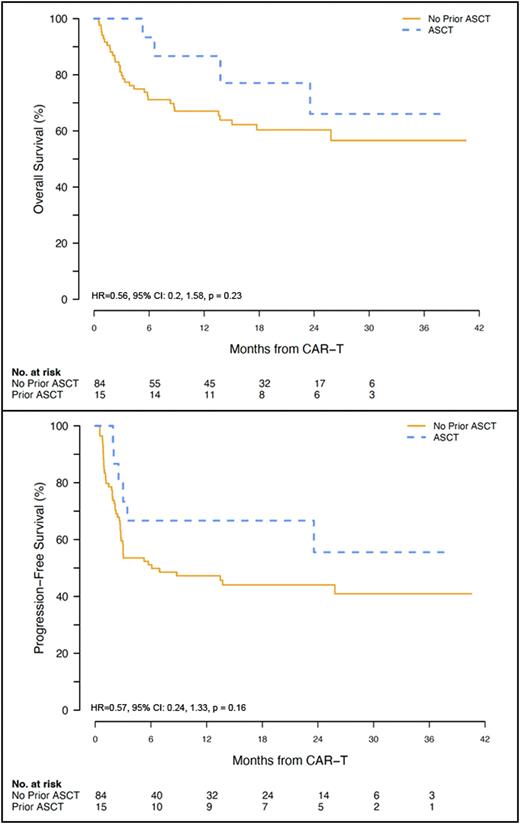
Methods Data was collected on 99 patients who received first axi-cel CAR-T therapy at our center for r/r DLBCL between 2018-2021. Of these patients, 84 were transplant naïve and 15 had received prior ASCT. We examined the rate of relapse/progression after CAR-T. Overall survival (OS) was defined as time from date of CD19 CAR-T therapy to death, censored at last known alive. Progression-free survival (PFS) was defined as time from date of CD19 CAR-T therapy to time of disease recurrence or death from any cause, censored at last known alive. Non-relapsed mortality (NRM) was defined as death without relapse or progression.
Results 63 patients (64%) were alive as of end of study date. Median follow-up time was 1.70 years (95% CI: 1.54-2.07) for all patients, 1.63 years (95% CI: 1.50-1.99) for transplant naïve patients, and 2.21 (95% CI: 1.09-not reached) for previously transplanted patients. 90-day disease response to CAR-T (CR, PR, SD and PD) was not different for transplant naïve vs. previously transplanted patients (P=0.444). Median OS was not reached for either transplant naïve or previously transplanted patients, with 2-year OS rates of 60% (95% CI: 50-73%) vs. 66% (95% CI: 43-100%) for previously transplanted patients (P=0.23). Median PFS was 0.51 years for transplant naïve patients and not reached for previously transplanted patients, with 2-year PFS rates of 44% (95% CI: 34-56%) for transplant naïve and 56% (95% CI: 33-92%) for previously transplanted patients (P=0.16). 2-year cumulative incidence of relapse or progression was 43% (95% CI: 33-54%) for transplant naïve and 33% (95% CI: 8-58%) for previously transplanted patients (P=0.43). 2-year NRM was 12% (95% CI: 5-20%) for transplant naïve and 11% (95% CI: 0-33%) for previously transplanted patients (P=0.44).
In multivariate analysis, bridging therapy, elevated LDH >600 at the time of lymphodepleting chemo, and grade 3 and 4 CRS were associated with worse OS; platelets <75,000 at the time of lymphodepleting chemo, grade 3 and 4 CRS and elevated LDH >600 were associated with worse PFS. There was no difference in the incidence of high grade CRS and neurotoxicity, ICU transfer rate, cytopenias and length of hospitalization between the 2 groups.
Conclusions This study showed no significantly significant differences in the OS, PFS, relapse/progression and NRM of r/r DLBCL patients who received CD19 CAR-T-cell therapy (axi-cel) with or without prior ASCT. Other factors such as bridging therapy, elevated LDH and high grade CRS were associated with worse OS. We conclude that prior ASCT does not appear to adversely affect the outcomes of CAR-T-cell therapy.
Disclosures
Yared:Kite: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal